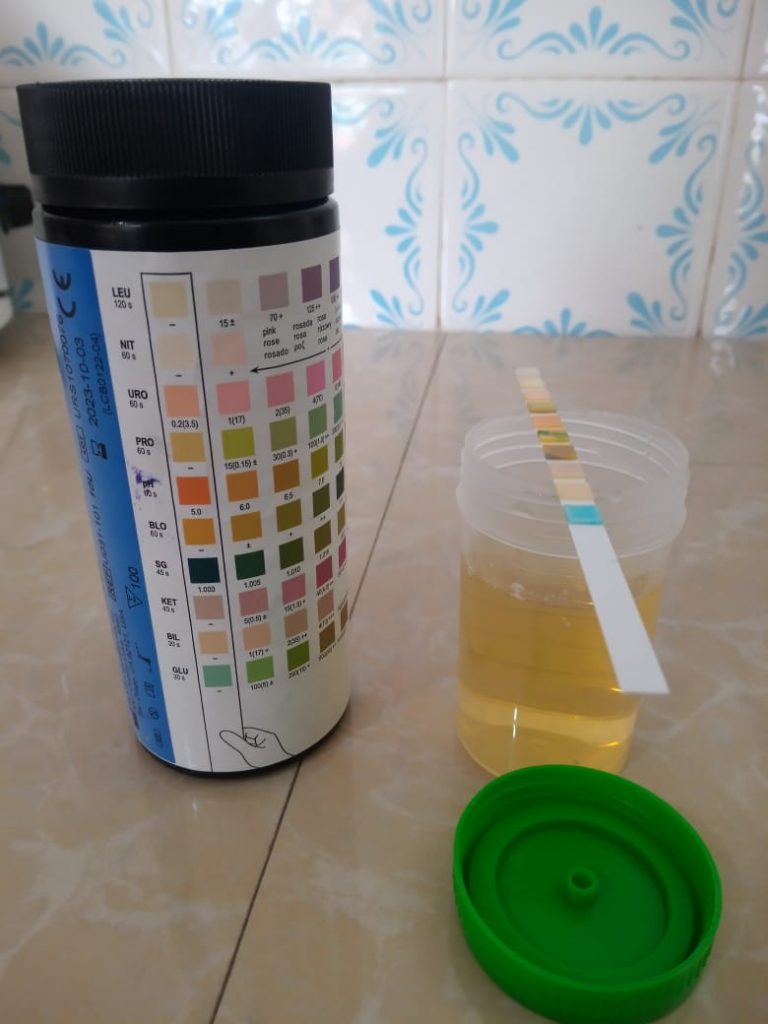
The urine dipstick test is commonly known as urinalysis. It is among the most common and affordable tests yet it is often underutilized. The secret to optimally utilizing the urine dipstick test is to learn to interpret its results. The urine dipstick comprises 11 chemical tests. The tests are useful in the diagnosis of multiple conditions such as urinary tract infections, diabetes insipidus, uncontrolled diabetes mellitus, and many more. The aim of this article is to give healthcare providers insights on how to optimally use the urine dipstick to diagnose urinary tract infections (UTIs).
Just like any other test, the best way to interpret results is to analyze them based on the suspected conditions. When a clinician takes the history of a patient and conducts a physical examination, he/she makes a presumptive diagnosis. The preliminary diagnosis should give the general orientation when interpreting results. A clinician who orders a test without having a presumptive diagnosis is like a researcher who starts collecting data before stating the research hypothesis.
Let’s consider a scenario where a physician or a nurse practitioner orders a urine dipstick test after making an “uncomplicated acute UTI” presumptive diagnosis in an adult non-pregnant patient. The clinician’s aim in diagnosis is to know whether the patient has bacteriuria, identify the uropathogen causing the UTI, and determine its antibiotic susceptibility pattern for early initiation of targeted antibiotic therapy. The specific diagnosis is important because the empirical treatment based on presumptive diagnosis is associated with an increased incidence of antimicrobial resistance.
The gold standard for making the specific diagnosis is urine culture and antimicrobial sensitivity. However, urine culture and sensitivity take a minimum of a day to conduct. In some healthcare facilities, the test may not be even available. In most instances, clinicians have no option but to administer empirical antibiotic treatment despite the risk of antimicrobial resistance.

An alternative of using rapid tests developed to detect bacteriuria or bacterial activity in urine is emerging. An example is the Micro Biological Survey (MBS) Point of Care Test (POCT). It is a culture-based method that detects bacteria and assesses the concentration of viable bacteria in the urine. It measures the activities of enzymes involved in bacterial metabolism to determine the bacterial concentration in urine in less than six hours.
However, since MBS-POCT does not identify bacteria, it can only be valuable if used alongside another test such as Matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry analysis for the identification of causative bacteria. Therefore, the rapid diagnosis of UTIs may not be currently affordable in resource-limited settings.
Clinicians without access to the new rapid tests such as the MBS-POCT and MALDI-TOF analysis can leverage a combination of signs and symptoms and urine dipstick test results to predict acute uncomplicated UTIs. The clinical providers need knowledge of recent research findings for evidence-based predictions.
Hematuria, dysuria, frequency, urgency, nocturia, and dysuria are useful signs and symptoms in the prediction. When the signs and symptoms are interpreted alongside urinalysis results, the predictive power increases. For example, a systematic review of 16 research articles found that predicting a UTI based on the combination of the presence of hematuria and a positive nitrite test has a probability of more than 90% accuracy. Additionally, a combination of dysuria and a positive nitrite test has a probability of about 70% accuracy in predicting a UTI.
Other notable research findings regarding predicting UTIs include ruling out a UTI when a patient does not present with urgency, frequency, and dysuria. Secondly, a vaginal discharge in women decreases the likelihood of the patient having a UTI. Thirdly, the nitrite test compared to the leucocyte esterase test may be more useful in predicting UTIs when combined with the relevant signs and symptoms.
Notably, the healthcare provider has to know the most common causes of UTIs in their locality to identify the most appropriate antibiotics to administer based on the predicted diagnosis. Additionally, the professional ought to know the antimicrobial susceptibility patterns of the suspected uropathogens to ensure only effective antibiotics are prescribed.
Evidently, continuous professional education based on recent research findings is pivotal in improving the clinical utility of the urine dipstick to diagnose urinary tract infections and other conditions. You can engage MedRight Consulting LTD to train your healthcare professionals to optimally use the urine dipstick test in clinical diagnosis.

Leave A Comment